
By Ellen N. Woods
CatholicU, Fall 2021
With the coronavirus raging in early 2020, Biology Professor Venigalla Rao brought 40 years of research on one tiny virus to bear in the urgent quest for a vaccine. He found rapid success in animal studies. Now his vaccine is headed to clinical trials.
In 2019, Biology Professor Venigalla Rao was working on an exciting project — development of a universal flu virus vaccine. He had submitted his grant proposal to the National Institutes of Health (NIH). “We were looking at designing a universal vaccine template that can be adapted quickly to any emerging pathogen,” says Rao. “We were going to use flu as the model."
If it worked, this would be a game changer. The needle-free nasal spray would be easier to produce and administer, be more cost-effective, and have the potential to protect against most variants of the flu virus with long-term protection.
This was no pie-in-the-sky endeavor. Rao’s proposal was based on more than 40 years of research related to one tiny, complex, benign virus: bacteriophage T4. The virus is called a bacteriophage because it infects bacteria, namely E. coli, the harmless bacteria that live in our guts.
Rao’s work studying the genetics and atomic structures of the virus at its most basic level has led to significant breakthroughs in the discovery of the function, mechanism, and biomedical application of phage T4, ultimately leading to outcomes that show how this microorganism could be used as a vehicle to carry innovative new vaccines and gene therapies into the human body.
When word started to come from Wuhan, China, of a SARS-CoV-2 virus causing pneumonia-like symptoms, Rao paid attention. As the number of cases was increasing, along with the severity of illness, he knew he had to change the focus of his research project.
In early January 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) a public health emergency worldwide.
“As a virologist, it was clear to me that this was a dangerous and highly transmissible virus,” says Rao. “It was very different from the previous SARS [Severe Acute Respiratory Syndrome]. There would be no way its spread around the world could be stopped. We knew we needed to do something. We had the bacteriophage platform and the technology to incorporate any pathogenic material into a vaccine. We had also recently developed a powerful CRISPR genome technology that allows us to engineer the virus in an accelerated fashion.”
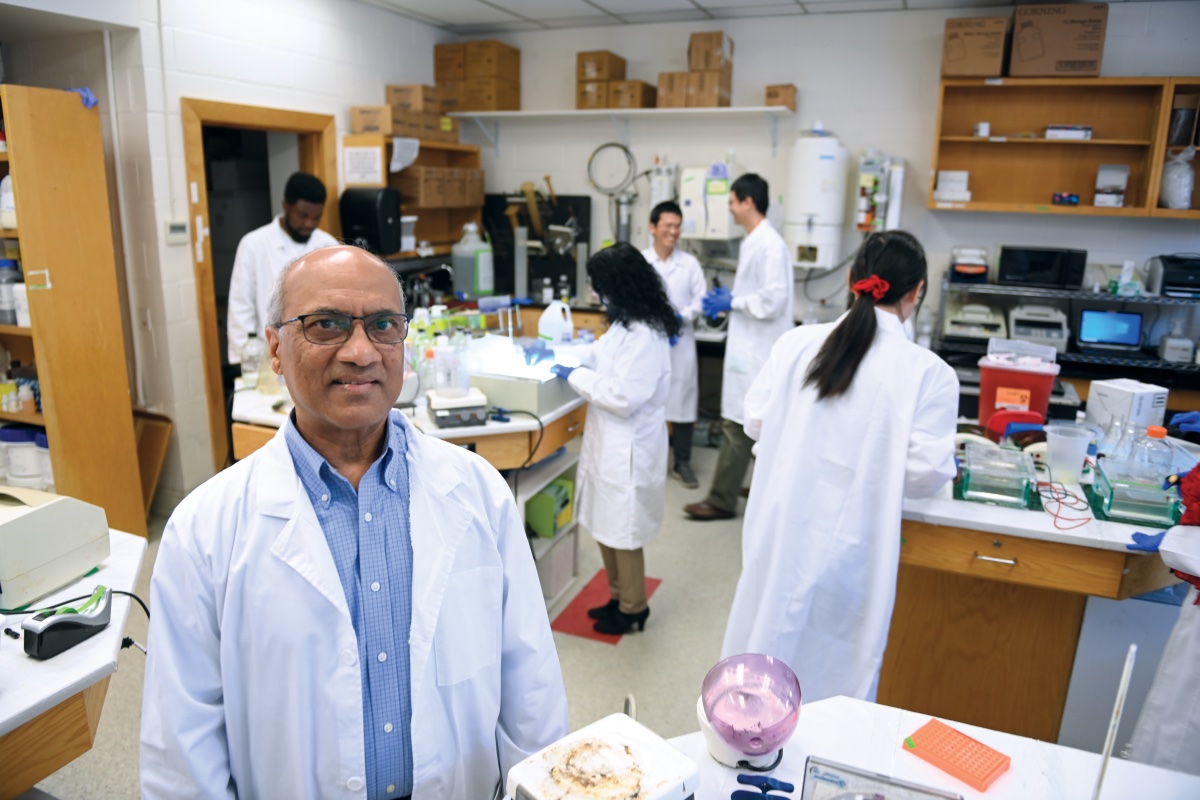
In late January, Rao assembled the members of his research team — Ph.D. students and post-doctoral researchers who share his passion for the study of bacteriophage T4 and its therapeutic value — in a meeting room on the third floor of the McCort-Ward biology building. Standing in front of a blackboard, Rao picked up a piece of chalk and, borrowing the line synonymous with the Apollo 13 space mission, wrote, “Failure is not an option.”
All were onboard with suspending their existing research projects and directing the resources toward designing COVID-19 vaccine candidates. Their quest would prove more intense than they could have imagined.
Rao’s love of science began at an early age. He was raised in Donepudi, a small village in Andhra Pradesh, India. His chore was to cut grass and haul it on the back of his bicycle to feed the buffaloes on his family’s small farm. He rode that same bike 10 miles each way to attend college, which begins after 10th grade in India. He had a chemistry teacher who recognized his aptitude for science and invited Rao to join his tutoring group. That mentorship helped him earn a scholarship to pursue a master’s degree in biochemistry at Andhra University.
Later, he would travel 500 miles by coal train from his family’s home to begin a Ph.D. program at the prestigious Indian Institute of Science in Bangalore. Rao earned his doctorate in five years with a dissertation on enzyme engineering. The day after submitting his thesis, he took his first- ever plane ride, traveling to Baltimore to begin a post-doctoral fellowship at the University of Maryland School of Medicine in the lab of Professor Lindsay Black, “an excellent mentor,” who was studying bacteriophage T4.
Reflecting on his nine-year fellowship (1980–1989), Rao says he was introduced to what would become his life’s work and passion, “the amazing world of bacteriophages.” He started with a challenging goal — to assemble the bacteriophage T4 virus in a test tube. It would take him seven years.
Rao is credited with discovery of the bacteriophage T4 DNA packaging machine. When he began his research more than 40 years ago, little was known about the virus genome packaging or the machinery involved in carrying out its complex process. Rao, as lead author, and Black published several key papers during that time describing the packaging machine, the capsid (protein shell of a virus, enclosing its genetic material), and the motor.
In 1989, Rao joined Catholic University’s Department of Biology as an assistant professor. Soon after, he received a Department of Energy grant. His curiosity about, and dedication to, T4 never wavered even though it would be a few more years before he would see another grant. He continued to publish and build a research lab around the virus, and the grants eventually followed.
In addition to the discovery of the DNA packaging machine, Rao has continued to make history in the field of virology with the discovery of the functional motifs that power the packaging machine, the atomic structures of the machine, and the dynamic inner workings of single packaging machines in real time.
Rao and his collaborators established that the phage T4 motor is the fastest and most powerful packaging machine known. The motor would be twice as powerful as an automobile engine if it were scaled to that size. The actual size of the motor is 17 nm wide and 9 nm high. (One nanometer is equal to one millionth of a millimeter.) The bacteriophage’s packaging machine allows it to reproduce within a host bacterium by rapidly pulling a long strand of DNA into a tiny shell the bacteriophage manufactures.
“These powerful engineering concepts have allowed us to develop T4 as a nanoscale device that can deliver pathogen antigens and gene therapeutics into human cells,” says Rao. This is done by decorating the outer surface of the capsid with proteins and complexes, while the interior is packaged with therapeutic DNA molecules. The development of a CRISPR phage engineering strategy is one of Rao’s most recent research achievements, allowing for the rapid construction of recombinant phages for vaccine and gene delivery.
“We are using the T4 virus’s own strategies for beneficial applications, such as engineering it to mimic another virus or pathogen. Simply put, our immune system recognizes the engineered T4 virus as a pathogen and elicits immunity against it,” says Rao. “We can also engineer the DNA-packaging nanomotor to make it deliver therapeutic molecules into targeted cells to treat genetic diseases such as sickle cell disease or cancer.”
Rao, an elected fellow of the prestigious American Academy of Microbiology, has documented his work in 120 peer-reviewed articles in such respected scientific journals as Cell, Science Advances, Nature Communications, and Proceedings of the National Academy of Sciences.
He has received more than 20 grants, most notably from the National Science Foundation, the NIH, and the Department of Defense (DoD). His discoveries have resulted in 23 patents for the University. The break-throughs have led to biomedical applications of phage T4, including the design of a dual anthrax-plague vaccine, that affords complete protection against two deadly bioterror agents.
“Dr. Rao took the study of T4 to a new level. No one else has thought to reconstruct this infectious organism in such a way to use it for a whole variety of beneficial applications,” says Frank Maldarelli, an NIH clinical investigator who heads the Clinical Retrovirology Section at the HIV Dynamics and Replication Program of the National Cancer Institute. He and Rao have collaborated on HIV vaccine research.
“To say that he thinks outside the box would not be accurate because for Rao, there is no box. He does not acknowledge a system of barriers. The possibilities for his research are as endless as his imagination,” says Maldarelli.
A life’s work of discoveries perfectly positioned Rao to join scientists around the world in the quest for COVID vaccines. With the platform well established, he would need the virus’ genetic material to get started. In February 2020, Rao reached out to contacts and collaborators, including Anthony Fauci, director of the NIH’s National Institute of Allergy and Infectious Diseases. Through material transfer agreements, he obtained the biologically safe nucleic acid codes for SARS-CoV-2 from both the NIH and the University of Texas, Austin.
As the team geared up by designing several different constructs for vaccine candidates, Rao wanted to find a way to be of immediate assistance during the crisis. He worked with the provost’s office on a plan through which the University offered royalty-free licenses to the vaccine delivery-related patents resulting from his research to scientists embarking on their own urgent COVID vaccine research.
“In the race to mitigate the spread and devastating death toll, the generosity and sharing within the scientific community was a bright spot,” says Rao.
Collaboration with researchers in complementary areas of study has been “one of the most joyous aspects of my career,” says Rao. He has had long-standing relationships with researchers at The University of Texas Medical Branch (UTMB), Purdue University, the University of California (San Diego), the National Cancer Institute, and the Walter Reed Army Institute of Research (where he collaborates with his wife, Mangala Rao, who is chief of Adjuvant and Antigen Research at the Military HIV Research Program).
One of his most cherished collaborators passed away in 2019. Nobel-Prize nominated scientist Michael Rossman was Purdue’s Hanley Distinguished Professor of Biological Sciences. Among his discoveries, he solved the structures of many viruses and proteins using X-ray crystallography. In an instance of serendipity, one of Rossman’s grants that was active at the time of his death allowed NIH to provide emergency funding for Rao’s COVID vaccine research with the support and cooperation of Purdue University.
By spring 2020, the virus was spreading in the United States and the Catholic University research team was working 12- to 14-hour days, seven days a week. The researchers, consulting with University administration and using their knowledge of infectious disease, instituted a set of safety protocols — in effect creating their own bubble within the third-floor lab spaces. The six-member team worked in a socially distanced model. Even though they were on the same floor working in their labs, their interactions took place via Zoom.
As the country went into lockdown and fear became as rampant as the virus, the team had a moment of questioning the safety of leaving their homes and traveling to campus every day.
“It was a scary time,” recalls Rao. “It wasn’t so much concern for themselves, but their families were understandably worried about their safety. Ultimately, we concluded that we could not afford to put the experiments on hold.”
“Teamwork is powerful,” says Swati Jain, Ph.D. 2020, a doctoral student of Rao’s who completed her dissertation during the pandemic, and stayed on in the lab to work on the COVID vaccine project. “We all had a role to play, and we were committed to keeping each other safe. With Dr. Rao as leader, it was very motivating. He has a never-give-up attitude. His love of science and his care for his team are inspiring.”
“This was a once-in-a-lifetime chance as a scientist,” says Jingen Zhu, a post-doctoral fellow who worked on the design of the vaccine, specifically engineering the major components of the T4 phage. “The ultimate purpose of science is to serve people. We worked with an incredible sense of urgency, heart, and passion.”
“It is a golden moment when you know that you have the right skills and knowledge and the right platform to solve a problem that is happening around you in real time,” adds Jain.
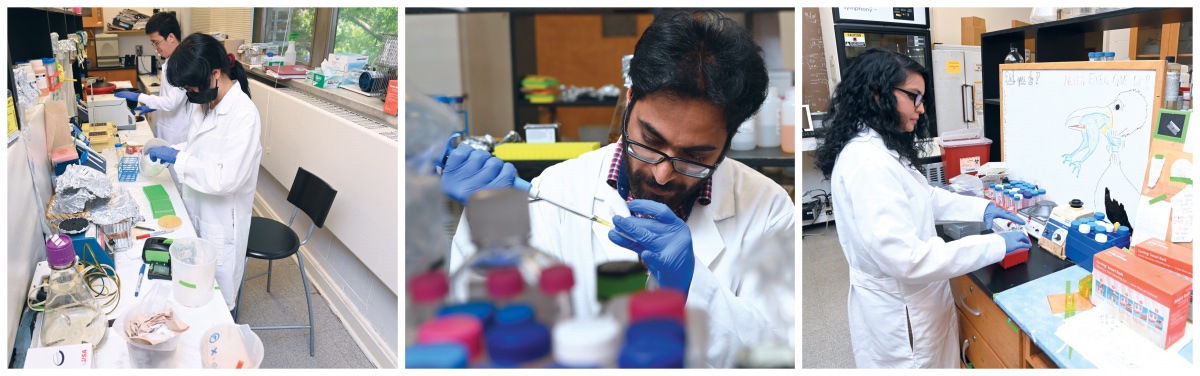 Members of the T4 vaccine research team at work in their labs: Jingen Zhu, Xiaorong Wu, Himanshu Batra, and Swati Jain. Members of the team not pictured are Neeti Ananthaswamy and Wei-Chun Tang.
Members of the T4 vaccine research team at work in their labs: Jingen Zhu, Xiaorong Wu, Himanshu Batra, and Swati Jain. Members of the team not pictured are Neeti Ananthaswamy and Wei-Chun Tang.
By October 2020, the team had found success. They had a vaccine candidate that produced strong antibody titers in immunized mice that completely blocked the infection of cultured cells by SARS-CoV-2 virus. Once they had this immunological data, the vaccine’s effectiveness needed to be tested with a lethal challenge to the mice with live SARS-CoV-2 virus, which would require a Biosafety Level 3 (BSL-3) facility.
Rao reached out to Ashok Chopra at the UTMB campus in Galveston, a researcher with whom he collaborated on the anthrax/plague vaccine. They worked out a plan to execute the challenge in Chopra’s BSL-3 laboratory.
Rao called it a “logistical nightmare,” and at the same time “a most generous act from fellow scientists.” The mice had to go through a series of protocols, including being tested for parasites, before UTMB could take the risk of accepting them. And a one-of-a-kind courier service had to be employed that had the expertise to ship 75 mice across the country. This meant keeping them healthy, warm, hydrated, and fed in a sterile, climate-controlled environment.
“It was one of the most anxiety-producing experiences of my life,” says Jain, who, with Himanshu Batra, Ph.D. 2020, worked directly with the mice throughout the study. “If anything happened to the mice, our entire study would be compromised.” On Nov. 20, the mice were in flight. When word came that they were diverted to Houston rather than the expected direct flight, the researchers held their breath, letting out a collective sigh of relief the next morning when the mice arrived at Chopra’s lab in good condition.
A few weeks later, Rao received the call he had hoped for. The immunized mice had survived the lethal challenge and were healthy. The weight of the control group of mice declined rapidly and within five days, 80% of them had died.
Adaptive Phage Therapeutics (APT), a clinical-stage biotech company focusing on advancing therapies to address drug-resistant infectious diseases, took note of Rao’s work. In August 2020, the company was awarded a $9.8 million DoD grant for research development of multiple high-priority, bacteriophage-based vaccine candidates against SARS-CoV-2. APT has partnered with Catholic University, conducting its own independent study of Rao’s platform, which confirmed the results.
Calling Rao “a pioneer in the use of phage as a vector for delivery of therapeutics and vaccines,” Greg Merril, APT’s CEO says, “We are focused on translating Dr. Rao’s amazing research into broad commercial availability. We believe the pre-clinical data is extremely promising and not just for COVID-19. His platform can be leveraged for other emerging variants and viruses as well.” (At press time, APT, working closely with Rao and his team, was expected to take the Catholic University vaccine to clinical trials in early 2022.)
In September 2021, “A Universal Bacteriophage T4 Nanoparticle Platform to Design Multiplex SARS-CoV-2 Vaccine Candidates by CRISPR Engineering” was published in Science Advances.
The article, published in record time in the world of scientific publication, documents the ways in which the T4 COVID vaccine differs from the vaccines that had come on the market in early 2021 through FDA emergency authorization. According to the abstract, the vaccine stimulated strong immune responses, blocked virus-receptor interactions, neutralized viral infection, and conferred complete protection against viral challenge. The T4 vaccine focuses on more proteins within the COVID-19 virus than do other vaccines, thus providing a broader and more robust immunity against the virus, and potentially against current and future variants.

In addition, the multi-component vaccine is adjuvant free (no chemicals), highly stable (possibly even at room temperature), cost-efficient to produce, and is being developed as a needle-free intranasal vaccine. These factors would make the vaccine especially useful in remote and disadvantaged countries, and for vaccinating children.
A few months prior to publication, when the research team members learned their paper had been accepted, they gathered in McCort-Ward Hall. With the availability of vaccines, they were just getting used to being together again. Rao brought a chocolate cake. Others brought homemade dishes. They celebrated in the room where the guiding words “Failure is not an option” have remained on the blackboard for 17 months. They don’t plan to pick up an eraser any time soon.